Do you suffer from swollen, painful, and restricted joint movements? Are you diagnosed with Osteoarthritis? If yes, then you should start taking treatment and should also self-educate yourself regarding this condition. After reading this blog you will be certainly able to answer the queries that you might have in your mind regarding osteoarthritis.
What is Osteoarthritis?
Osteoarthritis is a chronic progressive degenerative condition of the joints, meaning that the condition will deteriorate over time as it is a continuous process. Osteoarthritis affects mainly the articular cartilage of the big weight-bearing joints of the body mainly in aged individuals. It can be broadly classified into two types:- Primary Osteoarthritis
- Secondary Osteoarthritis
Secondary Osteoarthritis is due to abnormal wear and tear in a joint, caused by mechanical incongruity (lack of symmetry) of the articular surfaces. This incongruity may be the result of a preceding fracture involving the articular surface or partial destruction or deformity due to a previous disease. It can arise as a consequence of other conditions such as hyperthyroidism, dislocation, hemophilia, infection (tracking into a joint from an open wound) or tuberculosis of a joint, etc.
An osteoarthritic joint might be:
- Painful
- Swollen
- Stiff
- Tender on restricted movements
- Crackling or grating sound
- Bowlegs deformity (in later cases)
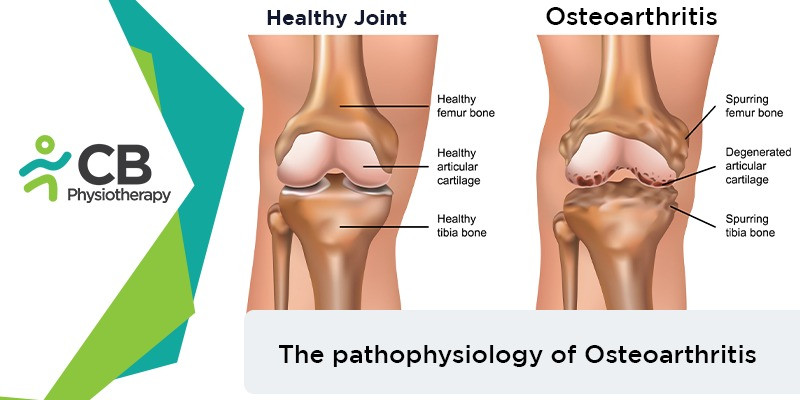
What changes take place in our joints due to osteoarthritis?
Articular cartilage of the surface
The place, where 2 bones meet, is normally covered with a rubbery material called cartilage. This material allows the bones to slide over each other without causing pain. When osteoarthritis sets in, the cartilage begins to break down and undergoes degeneration. As it is cyclically loaded during movements of joints, it undergoes fatigue failure leading to the fragmentation of the surface and fibrillation (cracks and fissures). In the later stages, the cartilage gets completely eroded, exposing the sclerosed or eburnated (hard and thick) bone and the subchondral cyst is also formed (Subchondral is the layer of bone just below the cartilage in a joint, chondral refers to cartilage. The subchondral bone is a shock absorber in weight-bearing joints. It has many blood vessels supplying it with nutrients and oxygen and taking away waste).Bone
The bone surfaces become hard and polished as they lose protection from the cartilage. Subchondral cysts and cavities are formed as the eburnated bones are brittle. Blood flow may be reduced by venous occlusion (blockage of a blood vessel) and the development of microemboli (small particles often a blood clot) in the subchondral vessels occurs.
And microfractures occur allowing the passage of synovial fluid into the bone tissue. There can be venous congestion (when arterial inflow is greater than venous outflow) also. The bone undergoes hypertrophy (increase in no and size) forming peripheral osteophytes (bony projections)
Synovial membrane
The synovial membrane undergoes hyperemia (excess blood in the vessels) dry and reactive inflammatory thickening. Reduction of synovial fluid secretion results in loss of nutrition and lubrication of the articular cartilage.
Capsule
There is degeneration of the capsule along with chronic inflammation.
Ligaments
Ligaments become contracted or elongated.
Muscles
Muscles undergo atrophy meaning muscle wasting due to loss of movement and function, as a result of pain
Joint space
Joint spaces become narrow and joints become stiff. The stiffness is maximum at the end of a long rest period and loosens for a few minutes during activity.
There is no permanent cure for osteoarthritis but with a good diet and exercise, you can stop the condition from progressing further. The management involves the role of Doctors, Dieticians, Pharmacists, Occupational therapists, and Physiotherapists.