Pelvic Floor Relaxation Techniques:
In cases of overactive pelvic floor muscles, relaxation techniques may be taught to reduce muscle tension and improve urinary symptoms.
Behavioral Strategies:
Physiotherapists may provide guidance on behavioral strategies such as bladder training, timed voiding, and fluid management to improve bladder control.
Electrical Stimulation (ES) or Neuromuscular Electrical Stimulation (NMES):
This involves the use of low-level electrical currents delivered through electrodes placed on or in the pelvic floor muscles. ES can help improve muscle strength, endurance, and coordination. It may also be used to address muscle overactivity in conditions like urge incontinence.
Intravaginal or Intrarectal Electrical Stimulation:
In some cases, electrodes are placed inside the vagina or rectum to provide more targeted stimulation to the pelvic floor muscles. This method can be particularly effective for strengthening specific muscle groups.
Biofeedback:
Biofeedback devices use electrical sensors to monitor muscle activity in real-time. Physiotherapists can use biofeedback to help patients visualize and understand how to engage and relax their pelvic floor muscles correctly. This can be a valuable tool for teaching proper muscle control.
Transcutaneous Electrical Nerve Stimulation (TENS):
While TENS is more commonly associated with pain management, it can also be used in the treatment of urinary incontinence. TENS units deliver low-frequency electrical impulses to the pelvic area to improve muscle function and reduce urinary symptoms.
Functional Electrical Stimulation (FES):
FES devices are designed to mimic natural muscle contractions. They can be used to stimulate the pelvic floor muscles to improve muscle strength and coordination.
Magnetic Stimulation:
Some physiotherapists use magnetic stimulation devices to stimulate the pelvic floor muscles. These devices use magnetic fields to induce muscle contractions and can be beneficial in cases of muscle weakness.
Interferential Current (IFC):
IFC is a type of electrical stimulation that uses two high-frequency currents to intersect within the body. It can help reduce pain and improve blood flow, which can be useful in combination with other therapies for pelvic floor rehabilitation.
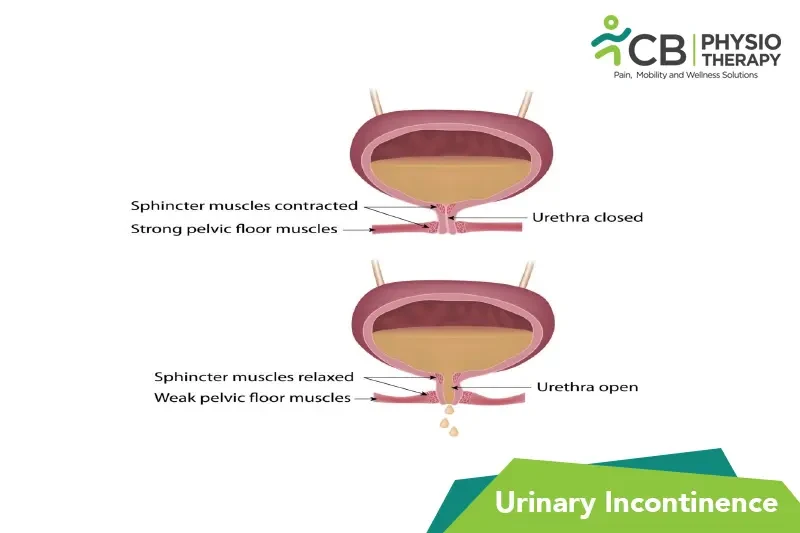
Pelvic Floor Muscle Training:
Pelvic floor exercises, commonly known as Kegel exercises, are a cornerstone of physiotherapy for urinary incontinence. These exercises involve contracting and relaxing the pelvic floor muscles to strengthen them.
Lifestyle Modifications:
Physiotherapists often offer advice on lifestyle modifications, including dietary changes, weight management, and exercises to support overall pelvic health.
Select your City to find & connect with our experts regarding Physiotherapy for Urinary Incontinence