Migraines are a debilitating condition that affects millions of people worldwide. Characterized by intense, throbbing headaches often accompanied by nausea, vomiting, and sensitivity to light and sound, migraines can significantly impact the quality of life. While medication is a common treatment approach, physiotherapy has emerged as a valuable, non-pharmacological option for managing migraine symptoms. This blog explores the nature of migraines and delves into how physiotherapy can be an effective part of a comprehensive migraine management plan.
What Are Migraines?
Migraines are more than just severe headaches. They are a complex neurological condition with a variety of symptoms and stages. A typical migraine episode can be divided into four phases: prodrome, aura, attack, and postdrome.1: Prodrome: This phase occurs hours or even days before the migraine attack. Symptoms can include mood changes, food cravings, neck stiffness, and increased urination.
2: Aura: About 25% of people with migraines experience auras. These are visual or sensory disturbances that usually precede the headache phase. They can include flashes of light, blind spots, or tingling in the face or hands.
3: Attack: The headache phase can last anywhere from a few hours to three days. The pain is often on one side of the head and may be accompanied by nausea, vomiting, and extreme sensitivity to light, sound, or smell.
4: Postdrome: After the headache subsides, individuals may feel exhausted, confused, or generally unwell for up to a day.
Physiotherapy as a Tool for Migraine Management
Physiotherapy, also known as physical therapy, involves a variety of techniques designed to improve physical function and alleviate pain. When it comes to migraines, physiotherapy can address several contributing factors and symptoms, providing relief and reducing the frequency and severity of attacks.
1. Addressing Musculoskeletal Issues
Many migraine sufferers have underlying musculoskeletal problems, particularly in the neck and upper back. Poor posture, muscle tension, and joint dysfunction can all contribute to migraine frequency and intensity. Physiotherapists can use techniques such as manual therapy, stretching, and strengthening exercises to address these issues.a) Manual Therapy: This involves hands-on techniques to mobilize and manipulate the muscles and joints. It can help to reduce muscle tension, improve joint mobility, and alleviate pain. For example, mobilization of the cervical spine can help reduce the frequency of cervicogenic headaches, which can sometimes be mistaken for migraines.
b) Postural Training: Poor posture can lead to muscle imbalances and tension in the neck and shoulders, which can trigger migraines. Physiotherapists can teach patients how to maintain proper posture through exercises and ergonomic advice, reducing the strain on these muscles.
2. Improving Blood Flow and Reducing Tension
Migraines are often associated with poor blood flow and increased muscle tension. Physiotherapy can help to improve circulation and reduce muscle tightness through various techniques.a) Massage Therapy: This can help to relax tight muscles, improve blood flow, and reduce stress levels, all of which can help to alleviate migraine symptoms. Regular massage therapy can also help to prevent the buildup of muscle tension that can trigger migraines.
b) Heat and Cold Therapy: Applying heat can help to relax tight muscles and improve blood flow, while cold therapy can help to reduce inflammation and numb pain. Physiotherapists can advise on the appropriate use of these therapies for individual patients.
3. Exercise and Physical Activity
Regular physical activity is known to have numerous health benefits, including the reduction of migraine frequency and intensity. Exercise can help to improve cardiovascular health, reduce stress levels, and improve overall physical function.a) Aerobic Exercise: Activities such as walking, swimming, and cycling can help to improve cardiovascular health and reduce stress levels, both of which can help to reduce the frequency and severity of migraines. Physiotherapists can develop individualized exercise programs that take into account the patient’s fitness level and any other health conditions.
b) Strength Training: Strengthening the muscles of the neck, shoulders, and back can help to improve posture and reduce muscle tension, which can help to prevent migraines. Physiotherapists can design specific strength training exercises that target these areas.
4. Stress Management and Relaxation Techniques
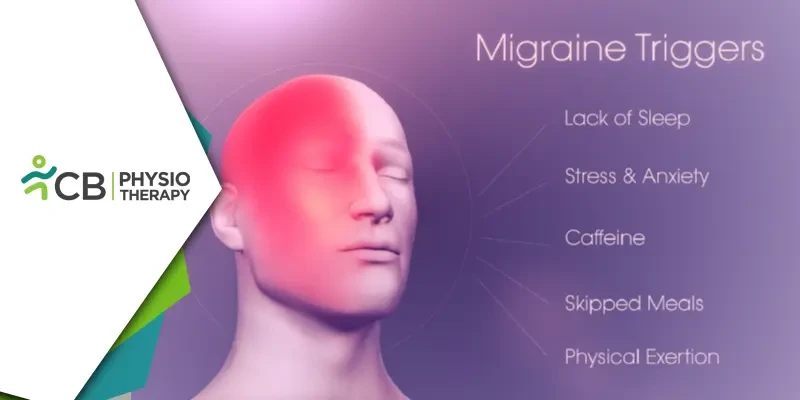
Stress is a well-known trigger for migraines. Physiotherapy can include various techniques to help patients manage stress and promote relaxation.a) Relaxation Techniques: Techniques such as deep breathing exercises, progressive muscle relaxation, and guided imagery can help to reduce stress levels and promote relaxation. Physiotherapists can teach these techniques and incorporate them into the patient’s overall treatment plan.
b) Trigger Identification and Avoidance: Physiotherapists can help patients identify and avoid common migraine triggers, such as certain foods, environmental factors, and stress. By keeping a migraine diary, patients can track their symptoms and identify patterns that may indicate specific triggers.
Migraines are a complex and often debilitating condition that can significantly impact quality of life. While medication is commonly used to manage symptoms, physiotherapy offers a valuable, non-pharmacological approach to migraine management.