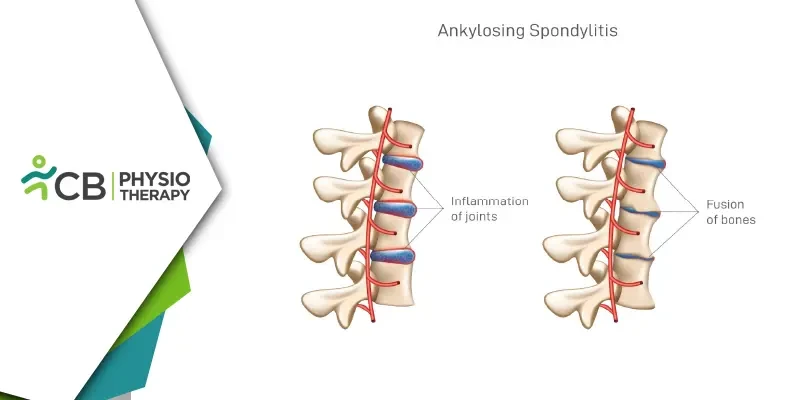
Ankylosing spondylitis (AS) is a chronic, progressive inflammatory disease that primarily affects the spine and sacroiliac joints, leading to pain and stiffness. It is part of a broader category of diseases known as spondyloarthropathies, which also includes conditions like psoriatic arthritis and reactive arthritis. AS typically begins in early adulthood and is more common in men than women. Over time, the inflammation can lead to the fusion of the vertebrae, causing a loss of flexibility and, in severe cases, a hunched-forward posture.
Ankylosing Spondylitis
The exact cause of AS is unknown, but it is believed to be linked to genetic factors, particularly the presence of the HLA-B27 gene. However, not everyone with this gene will develop AS, indicating that other factors, such as environmental triggers, may also play a role.The hallmark symptom of AS is chronic pain and stiffness in the lower back and hips, especially in the morning or after periods of inactivity. Other areas, such as the shoulders, knees, and ribs, may also be affected. As the disease progresses, the spine may become less flexible, and some individuals might develop a stooped posture. Inflammation of the eyes can occur, causing pain, redness, and blurred vision. If the ribs are affected, the chest's ability to expand may be limited, making breathing more difficult.
Role of Physiotherapy in Managing Ankylosing Spondylitis
Physiotherapy plays a vital role in the management of ankylosing spondylitis, helping to alleviate symptoms, maintain mobility, and improve the overall quality of life. The key physiotherapy approaches for Ankylosing Spondylitis include:1: Exercise Therapy
Regular exercise is one of the most effective ways to manage AS. A physiotherapist will develop a tailored exercise program based on the individual's needs and the severity of their condition. The program typically includes:
- Stretching exercises: Stretching helps to maintain flexibility and prevent stiffness in the spine and joints. Specific stretches may focus on the lower back, hips, shoulders, and chest to promote a full range of motion.
- Strengthening exercises: Strengthening the muscles that support the spine is essential for reducing the strain on the joints. Core strengthening exercises, such as planks and bridges, are often recommended to support the lower back.
- Cardiovascular exercises: Low-impact activities like swimming, cycling, and walking can improve cardiovascular fitness without putting excessive strain on the joints. Swimming is particularly beneficial as it combines cardio with resistance training in a low-gravity environment.
- Postural exercises: Postural training helps prevent or correct the stooped posture associated with AS. These exercises focus on the muscles of the back, neck, and shoulders to promote a more upright position.
2: Hydrotherapy
Hydrotherapy, or water-based therapy, is a popular modality for individuals with AS. The buoyancy of water reduces the weight-bearing load on the joints, making it easier to perform exercises with less pain and discomfort. The warm water can also help to relax tight muscles and alleviate stiffness
3: Manual Therapy
Manual therapy techniques, such as mobilization and manipulation, can help to reduce pain and improve joint mobility. These hands-on techniques involve the physiotherapist applying controlled pressure to the joints and soft tissues, helping to relieve stiffness and restore movement, but should be performed with caution,
4: Breathing Exercises
For individuals with AS, maintaining good lung function is essential, especially if the chest wall is affected. Breathing exercises can help to improve lung capacity and prevent the chest from becoming too rigid. Diaphragmatic breathing, which focuses on deep, slow breaths, can also help to reduce stress and promote relaxation.
5: Posture Correction
Physiotherapists work with individuals to correct posture, which is crucial for preventing or minimizing spinal deformities. This may involve ergonomic advice for daily activities, such as sitting, standing, and sleeping positions, as well as specific exercises to strengthen postural muscles. A posture correction program aims to maintain the spine’s natural curves and prevent the forward flexion often seen in advanced AS.
6: Pain Management Techniques
Physiotherapists can also provide pain management strategies, such as heat therapy, ultrasound, laser therapy and transcutaneous electrical nerve stimulation (TENS). These modalities can help to reduce pain and inflammation, making it easier for individuals to participate in exercise and daily activities.
Benefits of Physiotherapy for Ankylosing Spondylitis
The benefits of physiotherapy for individuals with AS are numerous and can have a profound impact on their overall well-being. Some of the key benefits include:1: Improved mobility: Regular exercise and stretching can help to maintain or improve the range of motion in the spine and other affected joints, preventing stiffness and maintaining functional independence.
2: Reduced pain: Exercise, manual therapy, and pain management techniques can help to alleviate pain and discomfort, making it easier to perform daily activities.
3: Enhanced posture: Postural exercises and education can help to prevent or correct spinal deformities, promoting a more upright and healthy posture.
4: Increased strength: Strengthening exercises help to build the muscles that support the spine, reducing the strain on joints and decreasing the risk of injury.
5: Better lung function: Breathing exercises can improve lung capacity and prevent the chest wall from becoming too rigid, ensuring good respiratory health.
Ankylosing spondylitis is a challenging condition, but with the right management strategies, individuals can lead active and fulfilling lives. Physiotherapy plays a crucial role in this management. Through regular physiotherapy, individuals with AS can achieve better control over their condition and enjoy a higher standard of living despite the challenges posed by the disease.