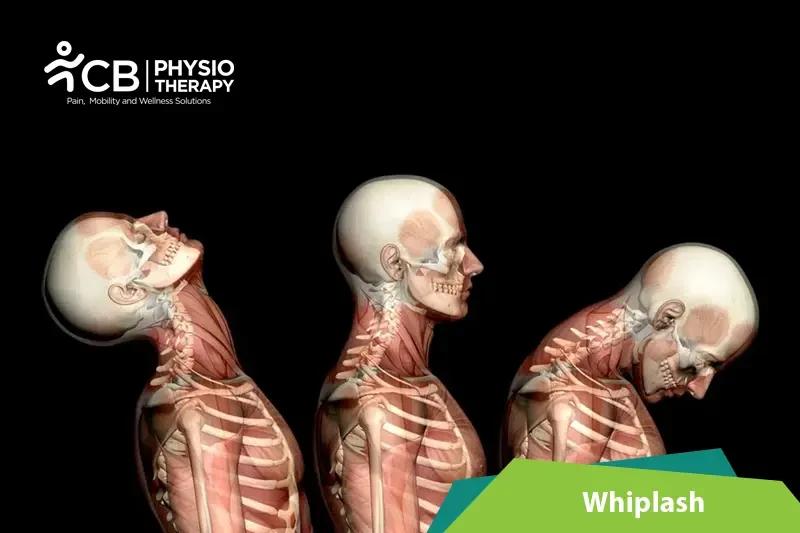
The term "whiplash" injury is used for accelerating-decelerating injuries that occur to the neck region or the cervical spine, modified to a term known as whiplash-associated disorders (WAD), these describe a collection of neck-related symptoms after a motor vehicle accident (MVA). Whiplash and whiplash-associated disorders (WAD) affect many structures of the cervical spine, depending on the force, the direction of impact, and many other factors.
The whiplash-associated disorder has a variety of motor, sensorimotor, sensory, and psychological symptoms some of them include:
Whiplash-associated disorders can occur due to no, of causes some of them are mentioned below:
Assessment of the patient with WAD should follow the normal cervical examination.
Physical examination:
Physical examination including inspection, palpation, ROM testing, and neurological examination is done to identify signs and symptoms of whiplash.
X-ray:
X-ray is recommended after the injury, a fracture, or damage to the spine. X-rays may also be used in patients whose symptoms don't improve after several weeks of injury.
Magnetic resonance imaging (MRI):
Magnetic resonance imaging, or MRI, is used to check the injury to the spinal cord or discs.
CT scan:
Computerized tomography, or CT scan, can show images of the bones and muscles.
Medication: Analgesics, nonsteroidal anti-inflammatory, muscle relaxants.
Note: Medication should not be taken without the doctor's prescription.
Therapeutic Ultrasound:
Therapeutic Ultrasound is recommended to promote healing and reduce pain, stiffness, muscle spasms and cramps.
Transcutaneous electrical nerve stimulation TENS:
Transcutaneous electrical nerve stimulation (TENS) may be used for the patient by applying a mild electric current to the skin. It helps to ease neck pain and improve muscle strength.
Ice therapy decreases the blood circulation in the injured part, which helps to reduce pain, inflammation, and muscle spasms.
Heat therapy increases blood circulation thus increasing the oxygen to the injured part. The blood removes the toxic substances which creates muscle spasms.
Rest:
Immobilize the neck for only a suitable time as prolonged immobilization may decrease muscle strength.
Soft foam:
Cervical collars can be used for whiplash injury to hold the neck and head still.
Range of motion exercises:
Early mobilization and range of motion exercises are most effective. Exercises like chin tuck help to retrain the deep muscles in the neck. After the car accident, the longus capitis and longus colli muscles of the neck have often decreased activity. Other exercises may include rotating the neck in both directions, tilting the head side to side bending the neck toward the chest, rolling the shoulders etc.
Strengthening exercises:
Strengthening the muscles, improves posture, and restores normal movement. Strengthening exercises like the serratus wall slide is a light strengthening exercise, it is a good re-training exercise for the serratus anterior muscle.
Stretching exercises:
Stretching exercises are done to increase range of motion, exercises like Levator release with a ball can be used to reduce muscle tightness where the shoulder and the neck meet.
The patient should be educated about motor vehicle accidents and advised to adhere to safe driving practices, like not driving while distracted, using seatbelts properly, and adjusting the headrest to the correct height.
Select your City to find & connect with our experts regarding Physiotherapy for Whiplash