Guillain-Barré Syndrome also known as G B Syndrome is a rare medical condition that triggers the immune system of the body to attack its nervous system, specifically the peripheral nerves that are responsible for sensation and motor control. This in turn affects the way brain signals are sent across the body and thus causes weakness, tingling, changes in sensations, and paralysis. Though there is no known cure for Guillain-Barré Syndrome. But, some treatments lessen the severity of the disease. Physiotherapy is one such treatment that plays a large role throughout the entire progression of Guillain-Barré syndrome. Physiotherapy does not affect the nerve healing process, it rehabilitates the muscles and works towards functional restoration and increasing stamina. This blog has been written to discuss exercises that help patients suffering from G.B Syndrome, to remain active and maintain strength.
GB Syndrome:
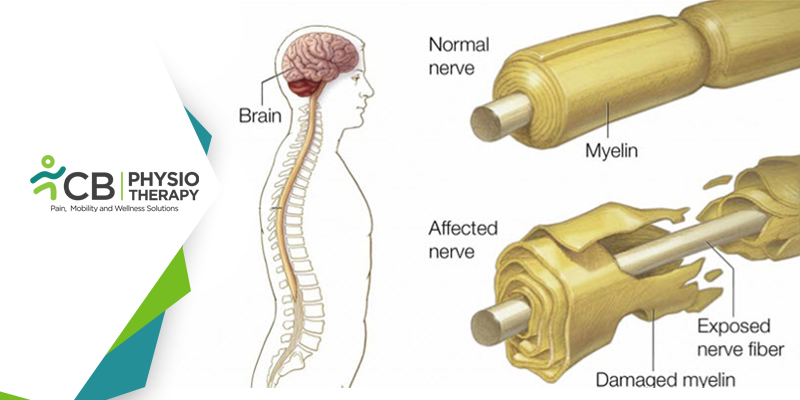
It is thought that GB syndrome occurs due to an autoimmune response after exposure to acute infections like a chest infection or diarrhea. It attacks the peripheral nerves and damages the myelin, an insulating layer of the nerve that is important in nerve impulse conduction. The patient has symptoms like feeling of altered sensation in the feet and hands, tingling and numbness in the fingers and toes, and progressive weakening of the limbs, legs, chest, hands, and arms spreading towards the trunk and face. This rapid progression of deterioration leads to the paralysis of muscle, sensory disturbances, respiratory difficulties, and problems with swallowing and speech. Most people reach the stage of greatest weakness after two weeks of the onset of the disease and might require hospitalization and ventilation. GB syndrome patients usually have residual weakness after 3 years, reduced stamina, and exhaustion after a period of increased activity during the recovery phase.
Physiotherapy Exercises
Physiotherapy treatment for patients with G-B Syndrome should be started immediately and continued until maximum recovery. Physiotherapy rehabilitation aims to maintain joint ranges of movement, increase muscle strength, restore mobility and balance, and re-train the normal movement patterns that are necessary for normal function and independence. The treatment required depends on the extent of the disease progression and the areas of the body which are involved. 1: Respiratory Exercises:
In severe cases, respiratory physiotherapy may be required. For patients who need more care, mechanical ventilation and suctioning are provided. If the muscles of the chest and respiratory system are compromised and weakness or paralysis occurs in the chest, individuals will experience respiratory issues. Then physiotherapy will promote lung hygiene and respiration through positioning, breathing exercises, secretion clearance, and manual chest physiotherapy techniques2: Exercises:
During the rehabilitation process, the patient suffering from G-B Syndrome is taught to use the energy constructively. This can be achieved by using the body correctly, avoiding unnecessary routines, and compensating for difficult activities by doing them another way. Passive limb movements to maintain joint ranges of movement and muscle flexibility while immobilization is recommended. Later, as the patient begins to recover physiotherapy is vital in assisting the restoration of muscle strength, limb control, balance, and coordination.3: Range of Motion exercises:
A: Ankle joint ROM exercises:The patient is made to sit on the floor with legs straight. Wrap a towel around the feet. And hold both ends of the towel in your hand. For ankle dorsiflexion gently point the toes toward the body, and slowly return to starting position, for ankle plantar flexion, point the toes away from the body, eversion of the foot is, by moving the foot outwards, inversion of the foot is by moving the foot inwards, and ankle circumduction of the foot, is by moving the foot in a circular motion.
2: Knee joint ROM exercises:
The patient is positioned supine lying for heel slides, bend the hip and knee by sliding the heel up toward the buttocks while keeping the heel on the bed. Slide the heel back down to the starting position and relax. Use a plastic bag under the heel to slide it easily.
3: Hip joint ROM exercises:
The patient is positioned supine lying for hip flexion, move the leg by sliding with knees straight, for leg slides ( hip abduction ) slide the leg out to the side, for adduction( Hip Adduction ) slide the leg back to the starting position, for hip extension, the patient is in standing position and push the leg towards the back.
4: Shoulder joint ROM exercises:
The patient is in a sitting position for shoulder flexion, raise the arm forward over up to the head, for shoulder extension bring the arm back to the side and return it to the starting position, for shoulder abduction raise the arm by the side and then up over the head as far as possible, for Shoulder adduction return the arm to the side, for shoulder rotation roll the shoulders in a smooth circle clockwise and anticlockwise.
5: Elbow joint ROM exercises:
Elbow flexion is done with the palm facing forward, just bending the elbow, and for the elbow, the extension returns the arm to the starting position.
6: Wrist joint ROM exercises :
Wrist flexion is done by bending the hand back towards the wrist so that the fingers point towards celling, for wrist extension bend the hand down so that the fingers points towards the floor, for wrist side to side movements move the hand from side to side, for wrist rotation roll the hand in circles clockwise and anticlockwise.
7: Hand and Fingers exercises:
Fingers bands make a tight fist and then relax it, for fingers spread open the hand and stretch the fingers as far apart as possible bring the fingers together again, for the finger to thumb touch, touch each fingertip with the pad of the thumb, for the thumb to palm stretch move the thumb across the palm.
8: Neck ROM exercises:
The patient is sitting or standing with the face forward shoulder should be straight and relaxed. For neck flexion gently bow down the head and try to touch the chin to the chest, for neck extension tilt the head back while looking towards celling, for neck side flexion tilt the head to the side and raise the shoulder, for neck rotations turn the head to look over the shoulder.
B: Strengthening Exercises:
1: Static quadriceps:Static quadriceps are done by tightening the muscles on the top of the thigh, by pushing the back of the knee down into the towel. Hold for 5 -10 secs and then relax.
2: Cat and Camel exercises:
The patient begins the exercise from 4 points kneeling, tucking in the chin, and rounding the back upward. Reverse by letting back one segment at a time, and keep the neck in neutral at the end. Hold 30 secs and repeat 3 times per session.
3: Bridging:
The patient is asked to lie on the back with knees bent and feet flat, and slowly lift the hips off. Hold for 5 - 10 secs and return. Make sure that the head and neck remain straight during the lift.
4: Knee to chest:
The patient is made to lie on the back with knees bent towards the chest. Wrap the arms around the legs to hold the hands in the position. Gently tuck the chin to the chest and hold the position for 30 secs, repeat 2 to 3 times.
5: Knee roll:
The patient is made to lie flat with knees bent and feet flat on the ground. Roll the knees side and stretch diagonally across the trunk. Bring back to the middle, and repeat the exercise over another side.
6: Chair stand:
The patient is asked to perform sit-to-stand exercises from the chair and repeat them 5 -10 times.
7: Gait Training:
A gait training program is given and gradually the distance of walking is increased.
Positioning:
Due to bed rest and prolonged sitting, pressure sores can develop. Physiotherapists ensure that proper bed positioning and continuous change in posture ensure that the risk is minimized. Physiotherapists also recommend the proper assistive devices such as orthoses and wheelchairs, if required.
Life Modification and Homecare:
The physiotherapist modifies the lifestyle of the patient to prevent contractures, DVT, and bedsores, and also support the weak extremities. Multiple rests between treatment sessions should be taken to reduce the level of stress by applying gentle massage to the affected area, maintaining a healthy weight, and doing regular physical activity. Individuals with Guillain-Barré Syndrome can also face emotionally painful periods as it is extremely difficult for patients to adjust to a state of sudden paralysis and dependence on others. The physiotherapy treatment plan can help through support and education as part of a holistic approach, and also advise patients about the help and support that can be provided through the use of other associated health professionals.The physiotherapist recognizes the body's signals and warnings when the patient's limit of exercise for that session is reached. These signals may include tingling, numbness, or other sensory abnormalities, pushing oneself through the limit can cause pain, weakness, spasms, and temporarily fatigued muscles. The patient must learn his/her limit, the need to rest as required and to interpret the body's signals and symptoms.