A quadriceps muscle strain is an acute tearing injury of the quadriceps, which usually occurs due to an acute stretch of the muscle and forceful contraction at the same time or repetitive functional overloading.
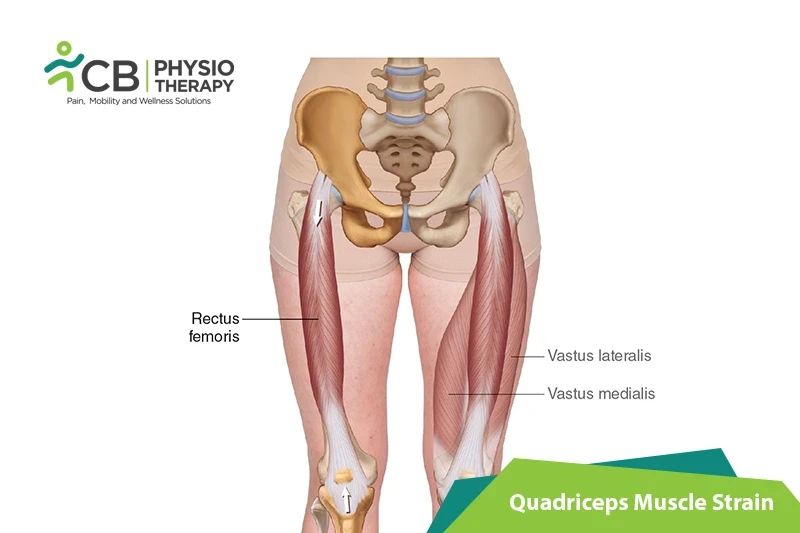
The Quadriceps femoris muscle is located in the anterior compartment of the thigh and is a hip flexor and a knee extensor. It consists of four parts:
Grades of Quadriceps Strain:
Grade 1: Grade 1 quadriceps strain is not always a serious injury. Spasm is at the site of injury and feeling of tightness and mild discomfort on walking and running might be difficult.
Grade 2: The patient feels a sudden sharp pain while running, jumping, or kicking and is unable to play. Difficulty in walking with swelling or mild bruising is present. Pain is felt while pressing in on the location of the quad muscle tear. Straightening of the knee against resistance causes pain and the patient is unable to fully bend the knee.
Grade 3: The patient feels severe, sudden pain in the front of the thigh and is unable to walk without a walking aid. Severe swelling appears immediately with bruising within 24 hours. Muscle contraction will be painful and can produce a bulge in the muscle.
Among quadriceps muscles, the rectus femoris is most frequently strained, due to reasons such as muscles crossing two joints, those with a high percentage of Type II fibers, and muscles with complex musculotendinous architecture. Acute injuries usually occur as a result of:
There is an increased risk of rupture due to a few medical conditions or due to the use of certain medications, including the following:
Symptoms of quadriceps strain depend on the type of injury, though common symptoms can be:
Pathology:
Strains are seen in all the quadriceps muscles but the rectus femoris is most vulnerable to strain as it passes over two joints: the hip and the knee. The most common site of strain is the distal musculotendinous junction of the rectus femoris. The patient feels a sudden pain in the anterior thigh during an activity requiring excessive muscle contraction. Other symptoms are local pain, tenderness, severe swelling, and bruising.
Physical examination:
After obtaining a thorough medical history, careful physical examination is done for observation, palpation, strength testing, and evaluation of motion.
The examiner has a close look at the affected area, observes swelling and bruising. Also, observes the patient in standing and walking, looks for postural abnormalities. Palpation of the quadriceps muscle is done along the entire length of the muscles. It's required to identify swelling, thickening, tenderness, defects, and masses if present. Strength testing of the quadriceps includes the resistance of knee extension and hip flexion. Adequate strength testing of the rectus femoris includes resisted knee extension with the hip flexed and extended. For this, the best way to evaluate the patient is in both sitting and prone-lying position. The prone-lying position allows optimum assessment of quadriceps motion and flexibility. Pain is usually felt by the patient with resisted muscle activation, passive stretching, and direct palpation over the muscle strain.
Ely's test:
The Ely's test is a physical test used to assess rectus femoris spasticity or tightness. The patient lies prone and the therapist stands next to the patient, at the side of the leg that is to be tested. One hand is placed on the lower back, the other hand holds the leg at the heel. Then flex the knee passively, the heel should touch the buttocks. For comparison test both sides. The test is positive if the heel cannot touch the buttocks, and the hip of the tested side rises from the table, the patient feels pain or tingling in the back or legs.
Radiographs:
Radiographs are effective to differentiate the etiology of the pain in the quadriceps muscles, which can be a muscular strain or stress fracture etc.
Ultrasound:
Ultrasound is often used as it is inexpensive. But it also has a disadvantage, that it's highly operator dependent and requires a skilled and experienced clinician. An advantage is that it can image the muscles dynamically and assess for bleedings and hematoma formation via Doppler.
Magnetic resonance imaging (MRI):
Magnetic resonance imaging (MRI) is used to give detailed images of muscle injury.
Medication: NSAIDs, pain killers, analgesics, etc.
Note: Medication should not be taken without the doctor's prescription.
Surgery:
Conservative treatment results in a good outcome. But there are certain specific indications in which surgical intervention might be beneficial, these are:
Rest:
Rest prevents worsening of the injury. Place the injured knee to rest the first few days after the trauma, this can prevent the formation of a large gap within the muscle, reduce the size of the hematoma, and the size of the connective tissue scar. A short period of immobilization accelerates the formation of granulation tissue at the site of injury during the initial phase. Gradually mobilization should be started to optimize the healing by restoring the strength of the injured muscle, preventing muscle atrophy, the loss of strength, and extensibility.
Ice therapy lowers the intra-muscular temperature and decreases blood flow.
Compression:
Compression wrap or bandage can help to decrease both blood flow and excess interstitial fluid accumulation. It aims to prevent hematoma formation and interstitial edema, thus decreases tissue ischemia.
Elevation:
The elevation of an affected leg above the level of the heart results in a decrease in hydrostatic pressure, and also reduces the accumulation of interstitial fluid, so there is less swelling at the place of injury.
Therapeutic Ultrasound:
Ultrasound helps to enhance the process of healing. It produces the thermal effect, which is of benefit to chronic muscle strains, it also reduces inflammation and promotes healing, which can help with an acute injury.
Transcutaneous electrical stimulation (TENS):
Transcutaneous electrical stimulation (TENS) can be used to decrease pain and swelling. It can help pump out inflammation, reduce pain, and desensitize nerve fibers. It also can strengthen muscle and re-educate.
Shockwave therapy is used to produce an improvement in healing and regeneration by a single acoustic wave impulse which stimulates healing of soft tissue, mainly by inhibiting the function of afferent pain receptors and increasing angiogenesis. Therefore, it increases blood flow by inducing a healing process mediated by the generated inflammatory process
Mobilization:
Mobilization is done to restore normal pain-free movement of the leg. The areas above and below the injury site are mobilized initially. It should be carried out gently and initially do not mobilize over the site of injury. But as the pain decreases, mobilization over adjacent sites to the injury can be started gently.
Active range of motion exercises:
Active range of motion is done once the injured leg is recovered well. This phase includes simple range of motion exercises like knee flexion extension, ankle movement, and toe movements. But before starting with AROM exercises passive movements are recommended.
Stretching Exercises:
Stretching exercises should be done carefully to the point of discomfort, but without pain. This includes techniques such as passive, active-passive, dynamic, and proprioceptive neuromuscular facilitation stretching. e.g. Static quad stretch, hip flexor stretch, etc.
Strengthening exercises are done to gradually increase the load that is put through a muscle. Initially, isometric or static exercises are advised, then progress to low-level pain-free exercises and then to advanced exercises with the resistance band and finishing with sports-specific running and sprint drills. Strengthening exercises can also be done in an aquatic pool by using the resistance of water.
Isotonic Exercise:
Isotonic exercises are begun with the lightest free weight, 3 sets of 10 repetitions up to 3 times a day. Terminal knee extensions at 20 degrees, increase as comfort and knee flexion allows. Once terminal knee extensions are done properly without extensor lag, free weights are added to the SLRs and terminal knee extensions, weight is increased slowly.
Eccentric Exercises:
These exercises include higher velocity eccentric exercises that include plyometric and sports specific activities such as squat jumps, split jumps, bounding and depth jumps, single leg bounding, backward skips, lateral hops, lateral bounding, plyometric box jumps, eccentric forward pulls, eccentric backward steps, eccentric lunge drops, single and double leg deadlifts, etc.
Isokinetic Exercises:
Isokinetic exercises are very high-intensity exercises such as swimming, running, treadmill walking Isokinetic strength testing should be performed under both concentric and eccentric action conditions.
The patient should be advised to do a proper warm-up and stretching before exercises or post-exercise. There should be a gradual increase in the exercise intensity or volume with complete monitoring. Complete rehabilitation programs should be followed in case of any injury to the lower limb.
Select your City to find & connect with our experts regarding Physiotherapy for Quadriceps Muscle Strain