मधुमेह से पीड़ित रोगियों में डायबिटिक फुट होता है, जो निम्न कारणों से होता है:
स्थिति की गंभीरता के आधार पर लक्षण अलग-अलग होते हैं। आमतौर पर पाए जाने वाले कुछ लक्षण हैं:
पैथोलॉजी:
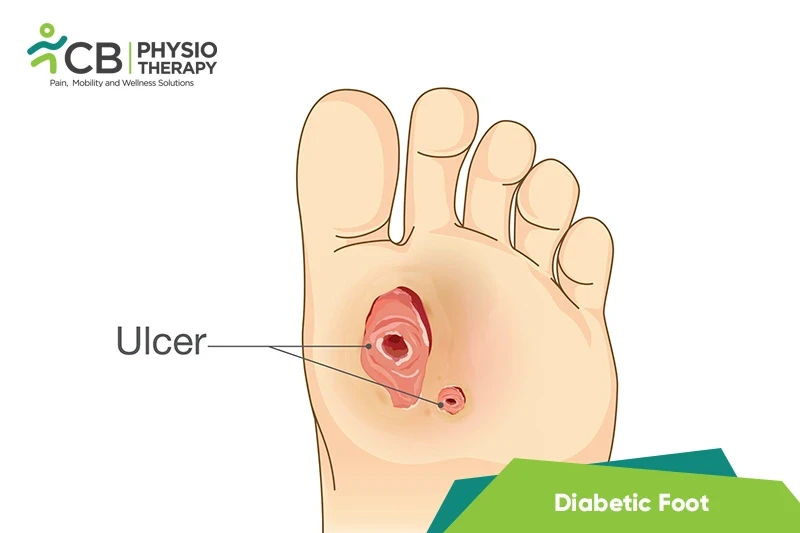
मधुमेह से संबंधित संवहनी रोग और न्यूरोपैथी के संयुक्त प्रभाव के परिणामस्वरूप मधुमेह पैर होता है, जो रक्त शर्करा के स्तर में लगातार उतार-चढ़ाव के कारण होता है, जिससे पूरे शरीर में नसों पर प्रतिकूल प्रभाव पड़ता है। केशिका तहखाने की झिल्लियों का मोटा होना, धमनी हाइलिनोसिस, और एंडोथेलियल प्रसार गंभीर मामलों में अल्सर का कारण बनता है।
शारीरिक परीक्षा:
परीक्षक लक्षणों की जाँच करता है, पैर की उंगलियों, पैरों या पैरों की जाँच करता है, और संवेदना या स्पर्श की अनुभूति की जाँच करता है। लाली, सूजन, गर्माहट, त्वचा का रंग उड़ना और त्वचा से निकलना जैसे संकेतों पर भी नज़र रखता है।
एक्स-रे:
एक्स-रे संक्रमण द्वारा हड्डियों को नुकसान के संकेतों की जाँच करता है, और गैंग्रीन जैसे नरम ऊतकों में विदेशी शरीर - एक बहुत ही गंभीर, जीवन-धमकी देने वाला, या अंग-खतरा करने वाला संक्रमण।>
डॉपलर अल्ट्रासाउंड:
निचले छोरों की रक्त वाहिकाओं पर एक गैर-आक्रामक जांच को घुमाकर, निचले छोरों में धमनियों और नसों के माध्यम से रक्त प्रवाह की जांच करने के लिए इसका उपयोग किया जाता है।
प्रयोगशाला परीक्षण:
संपूर्ण रक्त कोशिका गणना संक्रमण की उपस्थिति और गंभीरता को निर्धारित करने में मदद करती है। बहुत अधिक या बहुत कम WBC एक गंभीर संक्रमण का संकेत देता है। गुर्दे के कार्य परीक्षण, यकृत एंजाइम परीक्षण और हृदय एंजाइम परीक्षण का उपयोग यह आकलन करने के लिए किया जाता है कि गंभीर संक्रमण की स्थिति में अन्य शरीर प्रणालियां ठीक से काम कर रही हैं या नहीं।
दवा: Duloxetine, Pregabalin, एंटीबायोटिक, आदि।>
ध्यान दें: डॉक्टर के नुस्खे के बिना दवा नहीं लेनी चाहिए।< /अवधि>
सर्जिकल उपचार:
जब रूढ़िवादी उपचार मदद नहीं करते हैं या अपेक्षित परिणाम नहीं देते हैं, तो ऐसे मामलों में सर्जिकल उपचार का सुझाव दिया जाता है, जिसमें शामिल हैं:
<उल शैली = "सूची-शैली-प्रकार: डिस्क;">ऊंचाई के साथ बैंडिंग:
बैंडिंग ऊंचाई के साथ एडिमा को कम करने में मदद करती है।
मजबूत करने वाले व्यायाम:
मजबूत करने वाले व्यायाम मांसपेशियों की ताकत में सुधार करते हैं, मांसपेशियों को मजबूत और अधिक चोट प्रतिरोधी बनाते हैं और निरंतर प्रशिक्षण दिनचर्या के माध्यम से मांसपेशियों में खोई हुई ताकत हासिल करने में मदद करते हैं। हैमस्ट्रिंग, क्वाड्रिसेप्स, बछड़ा, और टिबियलिस पूर्वकाल की मांसपेशियों जैसी मांसपेशियों को मजबूत बनाने वाले व्यायाम की सिफारिश की जाती है।
चिकित्सीय अल्ट्रासाउंड:< /मजबूत>
अल्ट्रासाउंड एक अन्य प्रकार की फिजियोथेरेपी विद्युत पद्धति है जो त्वचा के नीचे ऊतक को उत्तेजित करने के लिए बहुत उच्च आवृत्ति ध्वनि तरंगों का उपयोग करती है। यह पैरों में संवेदनशीलता वापस लाने में मदद कर सकता है।
ट्रांसक्यूटेनियस इलेक्ट्रिकल नर्व स्टिम्युलेशन (TENS) ):
टेन्स कठोरता की भावना को कम करने में मदद करता है और पैर के छालों के उपचार को बढ़ाता है।
निम्न-स्तर लेज़र थेरेपी (LLLT) :
एलएलएलटी एक गैर-इनवेसिव, दर्द-मुक्त विधि है जिसे डायबिटिक फीट के लिए एक प्रभावी उपचार विकल्प माना गया है।
मसाज थेरेपी:< /मजबूत>
मालिश नियमित रूप से की जा सकती है। मालिश खराब रक्त आपूर्ति के कारण मांसपेशियों के संकुचन, ऐंठन और शोष को रोकता है।
गति अभ्यास की रेंज:
व्यायाम नियमित रूप से किया जाना चाहिए, क्योंकि वे न्यूरोपैथिक दर्द को कम कर सकते हैं और रक्त शर्करा के स्तर को नियंत्रित करने में मदद कर सकते हैं। यह सुनिश्चित किया जाना चाहिए कि डायबिटिक न्यूरोपैथी वाले लोगों के लिए व्यायाम करने से पैरों में चोट न लगे। हिप फ्लेक्सन, एक्सटेंशन, अपहरण, जोड़, आंतरिक रोटेशन, बाहरी रोटेशन, घुटने के फ्लेक्सन, एक्सटेंशन, एंकल डॉर्सिफ्लेक्सन, प्लांटरफ्लेक्सन, इनवर्जन और इवर्सन जैसे सक्रिय व्यायाम। साथ ही, कूल्हे और घुटने के सक्रिय सहायक व्यायाम की सिफारिश की जा सकती है।
स्ट्रेचिंग एक्सरसाइज:
स्ट्रेचिंग व्यायाम मैन्युअल रूप से किया जा सकता है। स्ट्रेचिंग एक्सरसाइज जोड़ों को लचीला बनाए रखने में मदद करती हैं और अन्य गतिविधियों के दौरान चोट लगने की संभावना को कम करती हैं। 5 से 10 मिनट तक हल्की स्ट्रेचिंग करने से शरीर को गर्म होने और चलने या तैरने जैसी एरोबिक गतिविधियों के लिए तैयार होने में मदद मिलती है। काफ स्ट्रेच, सीटेड हैमस्ट्रिंग स्ट्रेच और प्लांटर फेशिया स्ट्रेच स्ट्रेचिंग एक्सरसाइज के उदाहरण हैं।
बैलेंस ट्रेनिंग:
जोड़ों के दर्द, कमजोरी, या चक्कर आने के लिए संतुलन प्रणाली को स्वस्थ रखना महत्वपूर्ण है। संतुलन प्रशिक्षण सामान्य होने में मदद कर सकता है, और कठोरता या अस्थिरता की भावनाओं को दूर कर सकता है।
चाल प्रशिक्षण:
इस प्रशिक्षण में फिर से सीखना शामिल है कि कैसे चलना है और पैर की जटिलताओं, जैसे अल्सर और चोट को रोकना और स्थिर करना है। अंग खोने के बाद कृत्रिम अंगों का उपयोग करने वाले लोगों के लिए इस प्रकार की शारीरिक पुन: शिक्षा महत्वपूर्ण है यदि मधुमेह न्यूरोपैथी एक विच्छेदन की ओर ले जाती है।
एरोबिक व्यायाम
एरोबिक व्यायाम हृदय गति बढ़ाते हैं, मांसपेशियों का काम करते हैं, और श्वास दर बढ़ाते हैं। आमतौर पर, व्यक्ति दिन में लगभग 30 मिनट, सप्ताह में 3-5 दिन काम करता है। प्रारंभ में प्रतिदिन 5 या 10 मिनट के साथ शुरू करें और प्रत्येक सप्ताह समय बढ़ाते जाएँ। या दिन के लिए गतिविधि को विभाजित करें, प्रत्येक भोजन के बाद 10 मिनट चलने का प्रयास करें। एरोबिक व्यायाम के अन्य उदाहरण ट्रेडमिल पर तेज चलना, स्थिर साइकिल, कम प्रभाव वाली एरोबिक्स कक्षा, तैराकी, या जल एरोबिक व्यायाम हैं।
फिजियोथेरेपी के बारे में हमारे विशेषज्ञों को खोजने और उनसे जुड़ने के लिए अपने शहर का चयन करें डायबिटिक फुट