Neurogenic claudication, a term that may sound like medical jargon, is a condition that significantly impacts the quality of life for many individuals. This article aims to demystify neurogenic claudication, exploring its causes, symptoms, and the crucial role that physiotherapy plays in managing and alleviating its effects.
Understanding Neurogenic Claudication
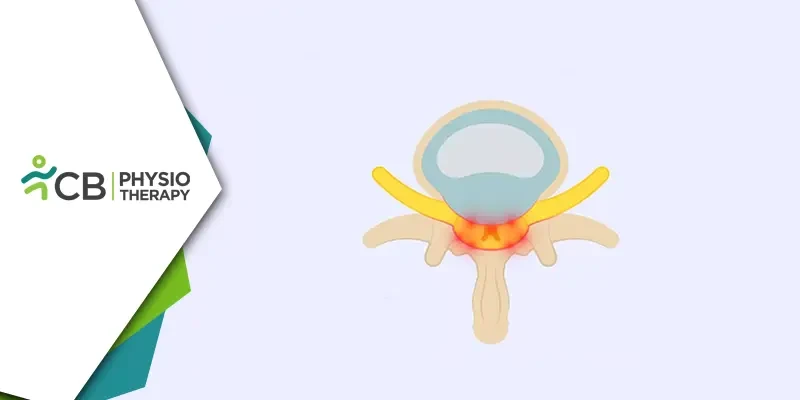
Neurogenic claudication is a type of claudication, a condition characterized by cramping, pain, or weakness in the legs, particularly during physical activity. Unlike vascular claudication, which is caused by reduced blood flow to the muscles, neurogenic claudication is rooted in nerve compression. The spinal canal, through which the spinal cord passes, may become narrowed due to various reasons, leading to compression of the nerves and subsequent symptoms.
Causes of Neurogenic Claudication
1: Spinal Stenosis: The most common cause of neurogenic claudication is spinal stenosis, a condition where the spinal canal narrows over time. This narrowing puts pressure on the nerves and can cause pain and discomfort.2: Herniated Discs: Discs in the spine act as cushions between vertebrae. When a disc herniates, the soft inner material protrudes, potentially compressing nerves and contributing to neurogenic claudication.
3: Degenerative Changes: Aging can lead to degenerative changes in the spine, such as the development of bone spurs. These changes can also contribute to the narrowing of the spinal canal.
4: Tumors: Rarely, tumors within or near the spinal canal can exert pressure on the nerves, causing neurogenic claudication.
The symptoms of neurogenic claudication typically manifest in the lower back, buttocks, and legs. Individuals with this condition may experience aching or sharp pain in the lower back and legs, especially during walking or prolonged standing. Some people may feel weakness or a heaviness in their legs. Sensations of numbness, tingling, or "pins and needles" in the legs may occur.
Understanding the Role of Physiotherapy
Physiotherapy, also known as physical therapy, plays a crucial role in managing neurogenic claudication. The primary goals of physiotherapy for this condition include pain relief, improving mobility, and enhancing overall quality of life.1: Pain Management: Physiotherapists may use modalities such as heat or cold therapy to alleviate pain and reduce inflammation. Hands-on techniques, including massage and joint mobilization, can help improve flexibility and reduce pain.
2: Strengthening Exercises: Building strength in the core muscles provides support to the spine, reducing the impact of nerve compression. Targeted exercises for the muscles of the legs can enhance stability and reduce symptoms.
3: Flexibility Training: Specific stretching exercises can improve flexibility and reduce stiffness in the affected areas, offering relief from neurogenic claudication symptoms.
4: Posture Correction: Physiotherapists provide advice on maintaining proper posture during daily activities to prevent exacerbation of symptoms. Teaching individuals how to move and lift properly reduces strain on the spine, minimizing the risk of nerve compression.
5: Gait Training: Physiotherapists may recommend assistive devices like canes or walkers to aid in walking, ensuring individuals can maintain mobility while minimizing pain.
6: Lifestyle Modification: Educating individuals about lifestyle changes, such as weight management and regular exercise, empowers them to manage their condition proactively.
Neurogenic claudication can be a challenging condition, impacting the daily lives of those affected. Physiotherapy emerges as a beacon of hope in managing and mitigating its effects. Through a combination of pain management strategies, targeted exercises, and educational initiatives, physiotherapists empower individuals to regain control over their lives. As research and advancements in physiotherapy continue, the future holds promise for improved outcomes and enhanced well-being for those grappling with neurogenic claudication.