Charcot-Marie-Tooth disease (CMT) is one of the most common inherited neurological disorders, affecting approximately 1 in 2,500 people worldwide. Named after the three physicians who first identified it in 1886—Jean-Martin Charcot, Pierre Marie, and Howard Henry Tooth—this disease primarily affects the peripheral nerves, which are responsible for transmitting signals between the brain, spinal cord, and muscles throughout the body. Over time, the disorder causes the muscles in the legs, feet, and hands to weaken and waste away, leading to difficulties with movement, balance, and coordination.
While CMT can’t be cured, physiotherapy plays a crucial role in helping individuals manage the symptoms, maintain their functional abilities, and enhance their quality of life. In this blog, we’ll explore the nature of Charcot-Marie-Tooth disease and how physiotherapy interventions can be used effectively to manage its progressive symptoms.
Understanding Charcot-Marie-Tooth Disease
CMT is part of a group of hereditary motor and sensory neuropathies. It’s caused by mutations in specific genes responsible for the structure and function of peripheral nerves. These nerves control muscles and relay sensory information like touch, pain, and temperature. When these nerves malfunction due to CMT, they can no longer transmit signals effectively, leading to muscle weakness, atrophy, and sensory loss.CMT is a slowly progressive condition, meaning symptoms tend to worsen gradually over time. The severity of the disease and the age of onset can vary widely, even among individuals with the same type of CMT. The two main forms of the disease are:
CMT Type 1: This type involves abnormalities in the myelin sheath, the protective covering that surrounds the nerves. Damage to the myelin sheath causes a reduction in the speed of nerve transmission.
CMT Type 2: This form involves damage to the axon, the long extension of the nerve cell responsible for sending electrical signals. This damage leads to a reduction in the strength of nerve transmission.
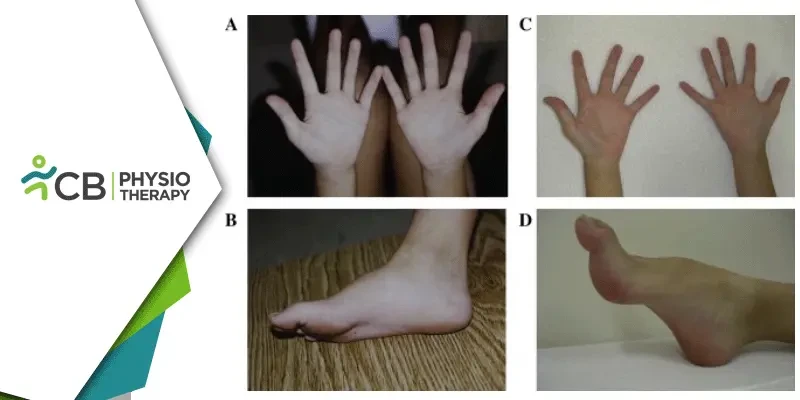
The symptoms of CMT include muscle weakness in the lower legs and feet, often leading to foot drop (difficulty lifting the foot while walking), high arches or flat feet, difficulty with balance and coordination, numbness or loss of sensation in the feet and legs, difficulty with fine motor skills, such as writing or buttoning a shirt, progressive muscle wasting, which can lead to difficulty walking or standing for extended periods
While CMT is not life-threatening, its impact on mobility, independence, and daily function can be significant, particularly as the disease progresses. This is where physiotherapy comes into play as a key intervention.
Role of Physiotherapy in Managing CMT
Physiotherapy is a cornerstone of the management of CMT. Since the disease affects both motor and sensory functions, the goals of physiotherapy are multifaceted. These goals typically include:1: Maintaining Muscle Strength: Physiotherapy exercises focus on preventing further muscle weakening, improving endurance, and preserving as much strength as possible in the affected muscles.
2: Improving Mobility and Gait: Individuals with CMT often experience gait abnormalities, such as foot drop or balance issues. Physiotherapists work to improve walking patterns through targeted exercises, gait training, and assistive devices.
3: Preventing Contractures and Joint Deformities: Prolonged muscle weakness can lead to contractures (stiffened joints) and deformities, such as high arches or hammer toes. Physiotherapy aims to maintain joint mobility and prevent these complications.
4: Enhancing Balance and Coordination: Since balance is often affected in CMT, physiotherapy can help individuals improve coordination and reduce the risk of falls.
5: Promoting Cardiovascular Health: Exercise programs are designed not only to improve muscle function but also to enhance cardiovascular fitness, which is essential for overall health.
Key Physiotherapy Interventions for CMT
Pain Management Although CMT is primarily a motor and sensory neuropathy, some individuals may experience neuropathic pain, especially as the disease progresses. Physiotherapy can help manage this pain through techniques such as:1: Massage and Soft Tissue Mobilization: These techniques can help alleviate muscle tightness and discomfort.
2: Transcutaneous Electrical Nerve Stimulation (TENS): This modality uses electrical stimulation to reduce pain signals and promote muscle relaxation.
3: Strengthening exercises are designed to target specific muscle groups affected by CMT. These exercises are typically low-resistance and high-repetition to avoid muscle fatigue. Common exercises include:
a) Ankle Dorsiflexion Strengthening: To combat foot drop, physiotherapists may focus on strengthening the muscles that lift the foot.
b) Toe Flexion and Extension Exercises: These help maintain the dexterity and strength of the toes, which are often impacted by the disease.
c) Leg and Hip Strengthening: Keeping the larger muscles of the legs and hips strong helps compensate for weakened lower leg muscles and improves mobility.
4: Stretching exercises help maintain flexibility, improve range of motion, and prevent contractures. Physiotherapists often recommend:
a) Calf Stretches: To maintain flexibility in the Achilles tendon, which can become tight due to foot drop.
b) Hamstring and Quadriceps Stretching: These muscle groups are important for maintaining balance and mobility.
c) Foot and Ankle Mobilizations: Gentle mobilizations can help prevent stiffness in the foot and ankle joints, particularly in cases of high arches or hammer toes.
5: Gait training aims to improve walking efficiency, reduce the risk of falls, and improve balance. This may include:
a) Assistive Devices: Physiotherapists may recommend ankle-foot orthoses (AFOs) to help support the foot and ankle and prevent foot drop. In some cases, walking aids like canes or walkers may be necessary.
b) Proprioceptive Training: To enhance sensory feedback and improve balance, exercises like standing on an unstable surface or using a balance board are incorporated into therapy sessions.
6: Aquatic Therapy For individuals with CMT, weight-bearing exercises can be challenging due to muscle weakness. Aquatic therapy is an excellent alternative, as the buoyancy of water reduces stress on the joints and muscles while still providing resistance for strengthening exercises. Water-based exercises also improve flexibility, balance, and cardiovascular fitness.
While Charcot-Marie-Tooth disease presents challenges in terms of mobility and physical function, physiotherapy offers a valuable and effective approach to managing the condition. By maintaining muscle strength, improving gait and balance, and promoting joint flexibility, physiotherapy helps individuals with CMT preserve their independence and quality of life for as long as possible. Early intervention and a personalized, progressive exercise program are key to optimizing outcomes and ensuring that individuals with CMT can continue to lead active, fulfilling lives.